Herd immunity, also known as herd immunity, occurs when a sizable percentage of a community is protected from an infectious disease because they have been immunised or have established immunity as a result of prior infection. Vaccination is preferred by the World Health Organization (WHO) over letting a disease to spread over any segment of the population, which could lead to more cases and deaths.
Protecting the public from the bacterium that causes COVID-19 through vaccination is preferable to exposing them to the disease itself in order to build herd immunity. For more information, please refer to the Director-speech General’s given at a media briefing on October 12.
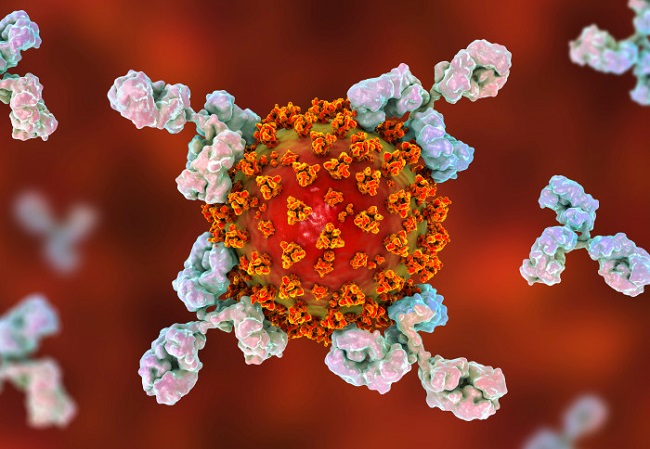
Vaccines, like natural exposure to a disease, prompt our immune systems to produce proteins that fight sickness (known as “antibodies”), yet unlike natural exposure, vaccines are effective without making us sick. Those who have been immunised are less likely to contract the disease and less likely to spread it to others, effectively stopping the spread of the illness. If you want to learn more about COVID-19 and vaccines, you may do so by visiting our dedicated website.
Many SARS-CoV-2 infected patients will likely continue to produce antiviral antibodies for the rest of their lives. Scientists’ findings of persistent antibody-producing cells in the bone marrow of COVID-191 survivors support this theory.
However, these cells quickly disappear once the virus has been eliminated, and other, more permanent cells produce antibodies: memory B cells monitor the blood for re-infection, and bone marrow plasma cells (BMPCs) remain dormant in the bones while secreting antibodies over the course of decades.
Ali Ellebedy, a B-cell immunologist at Washington University in St. Louis, Missouri, and the study’s lead author, says, “A plasma cell is our life history, in terms of the pathogens we’ve been exposed to.”
Last Words
All of the specialists agreed that those who have never received COVID-19 are unlikely to experience immunity in the same way those who have. In contrast to responding to a single viral protein provided by a vaccine, fighting a live virus is a unique experience. Those infected with COVID-19 also had six to twelve months to let the vaccine-induced immune response mature.
In contrast to someone who is inoculated and then re-immunized three weeks later, “those kinetics are different,” Pepper explained. “That’s not to suggest that they might not have as broad a response, but it could be very different.”


